Introduction to HIV & AIDS
Overview of HIV and AIDS
HIV (Human Immunodeficiency Virus) and AIDS (Acquired Immunodeficiency Syndrome) represent a significant public health challenge that has persisted since the virus was first identified in the early 1980s. HIV is a retrovirus that attacks the body’s immune system, specifically targeting CD4 cells, also known as T cells. These cells play a crucial role in the immune response, and their depletion leads to a weakened immune system. If left untreated, HIV can progress to AIDS, the most severe stage of HIV infection, characterized by life-threatening opportunistic infections or cancers due to the body’s diminished ability to fend off diseases.
The transmission of HIV occurs through specific bodily fluids, including blood, semen, vaginal fluids, rectal fluids, and breast milk. Understanding these transmission routes is essential for effective prevention strategies. The most common modes of transmission include unprotected sexual contact, sharing needles or syringes, and from an HIV-positive mother to her child during childbirth or breastfeeding. Awareness of these transmission vectors has played a pivotal role in the development of public health campaigns aimed at reducing new infections and educating communities about safe practices.
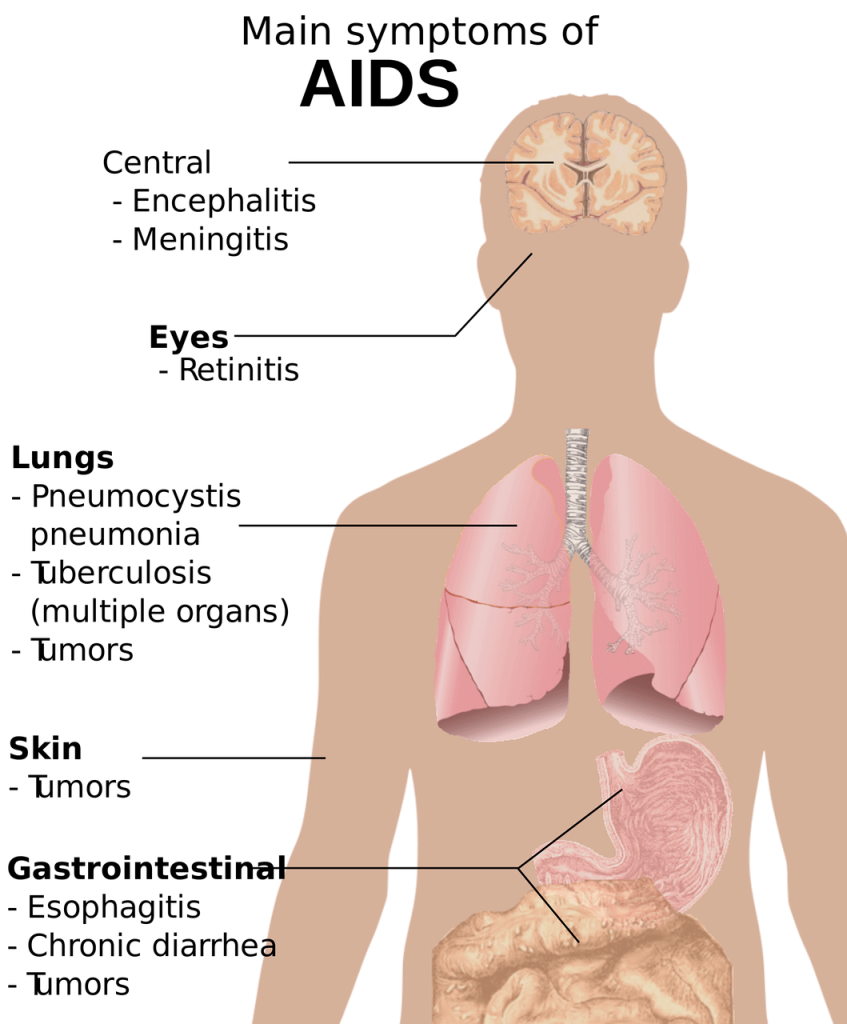
AIDS is diagnosed when an individual’s CD4 cell count falls below a certain threshold, or when they develop specific opportunistic infections or cancers associated with HIV. The progression from HIV to AIDS varies significantly among individuals, influenced by factors such as overall health, age, access to healthcare, and adherence to antiretroviral therapy (ART). With advancements in medical treatment, many people living with HIV can maintain their health and prevent the onset of AIDS through early diagnosis and consistent management of their condition.
The global response to HIV and AIDS has evolved over the decades, with significant advancements in treatment and prevention. The introduction of antiretroviral therapy has transformed HIV from a fatal diagnosis into a manageable chronic condition. Moreover, the concept of “Undetectable = Untransmittable” (U=U) has changed the conversation around HIV transmission, emphasizing that individuals who are on effective ART and maintain an undetectable viral load cannot sexually transmit the virus to others. This paradigm shift has empowered many living with HIV to lead fulfilling lives while also reducing stigma and fostering greater acceptance within society.
Despite the remarkable progress made in understanding and treating HIV and AIDS, challenges remain. Stigma and discrimination continue to affect individuals living with the virus, often hindering their access to healthcare and support. Additionally, certain populations, including men who have sex with men, people who inject drugs, and underserved communities, remain disproportionately affected by HIV. Continued education, advocacy, and research are essential to address these disparities and ensure that all individuals have access to effective prevention, treatment, and support services. By fostering a comprehensive understanding of HIV and AIDS, society can move closer to a future where stigma is diminished, and those affected can thrive.
Historical Context
The historical context surrounding HIV and AIDS is essential for understanding the disease and its socio-political implications. The first recognized cases of what would later be termed AIDS emerged in the early 1980s, primarily affecting young gay men in the United States. Initial reports from the Centers for Disease Control and Prevention (CDC) indicated a mysterious illness characterized by severe immunodeficiency, opportunistic infections, and certain types of cancers. The identification of these cases marked the beginning of a public health crisis that would not only challenge medical science but also expose significant societal prejudices.
In the years that followed, the epidemic spread rapidly, with HIV (Human Immunodeficiency Virus) being identified as the causative agent of AIDS (Acquired Immunodeficiency Syndrome) in 1983. The virus primarily transmitted through sexual contact, sharing of needles, and from mother to child during childbirth or breastfeeding, quickly gained notoriety. The association of HIV/AIDS with marginalized groups, particularly the LGBTQ+ community, led to widespread stigma and discrimination, complicating public health efforts. As fear and misinformation grew, so too did the need for advocacy and education, pushing affected communities to organize for their rights and for better healthcare resources.
The 1980s and 1990s were pivotal in shaping the response to the epidemic. Activist groups, such as ACT UP (AIDS Coalition to Unleash Power), emerged as powerful forces advocating for research funding, treatment accessibility, and the rights of individuals living with HIV/AIDS. Their relentless campaigns brought attention to the urgent need for effective therapies and public awareness. The challenges of the early years—characterized by inadequate medical responses and societal rejection—fostered a sense of urgency that ultimately propelled scientific inquiry and innovation in treatment.
The development of antiretroviral therapy (ART) in the mid-1990s transformed the landscape of HIV/AIDS management. These medications dramatically improved the prognosis for individuals living with HIV, turning a once fatal diagnosis into a manageable chronic condition. The introduction of ART also sparked discussions around prevention strategies, including the concept of treatment as prevention (TasP) and pre-exposure prophylaxis (PrEP). These advancements have not only improved individual health outcomes but have also fostered a shift in public perception and policy regarding HIV/AIDS.
Today, the historical context of HIV and AIDS serves as a reminder of the complexities involved in addressing public health crises. The lessons learned from the past highlight the importance of compassion, education, and inclusivity in health policies. While significant progress has been made in treatment and prevention, the enduring legacy of stigma and disparities in healthcare access remains a critical challenge. Understanding this history is vital for anyone engaged in the ongoing fight against HIV/AIDS, as it underscores the necessity for continued advocacy, research, and systemic change to ensure equitable healthcare for all affected individuals.
Current Global Statistics
The landscape of HIV and AIDS continues to evolve, presenting both challenges and opportunities in the global health arena. As of the latest reports, approximately 38 million people are currently living with HIV worldwide. This figure underscores the persistent prevalence of the virus, despite significant advancements in treatment and prevention strategies. The epidemic remains particularly concentrated in certain regions, with Sub-Saharan Africa bearing the highest burden, accounting for over two-thirds of the global total. Understanding these statistics is crucial for policymakers, healthcare providers, and communities aiming to combat the epidemic effectively.
In terms of new infections, around 1.5 million people were newly infected with HIV in 2021. This statistic highlights the ongoing transmission of the virus and the need for sustained prevention efforts. While there has been a decline in new infections since the peak in the late 1990s, progress has been uneven across different demographics and regions. Young women and adolescent girls, particularly in Sub-Saharan Africa, are disproportionately affected, with new infection rates among this group remaining alarmingly high. Addressing the unique vulnerabilities of these populations is essential for achieving global health goals.
The advancement of antiretroviral therapy (ART) has transformed HIV from a fatal diagnosis into a manageable chronic condition. Currently, approximately 28 million people living with HIV are receiving ART, which represents a significant increase from previous years. This treatment not only improves the quality of life for those infected but also reduces the viral load to undetectable levels, thereby minimizing the risk of transmission. However, despite these advances, a considerable gap remains, with nearly 10 million individuals unaware of their HIV status or unable to access treatment. Bridging this gap is critical for controlling the epidemic.
The global response to HIV and AIDS has also been influenced by the intersection of other health issues, such as tuberculosis (TB) and hepatitis. Co-infections with these diseases are prevalent among individuals living with HIV, complicating treatment regimens and health outcomes. The World Health Organization estimates that one in three people living with HIV also have latent TB infection, highlighting the necessity for integrated healthcare approaches. This statistic demonstrates the importance of addressing HIV not in isolation but as part of a broader public health strategy that considers the interconnectedness of various health challenges.
Finally, the impact of the COVID-19 pandemic has raised concerns about the future trajectory of HIV and AIDS responses worldwide. Disruptions in healthcare services, stigma, and economic downturns have hindered access to testing, treatment, and prevention programs. Preliminary data suggest that the pandemic may have led to an increase in new infections and a decline in treatment initiation rates. Moving forward, it will be crucial for global health initiatives to adapt and recover from these setbacks, ensuring that the progress made in the fight against HIV and AIDS is not lost. The current global statistics serve as a powerful reminder of the ongoing challenges and the collective effort required to overcome them.


No responses yet